The Sunshine Vitamin’s Dark Side: Safe Use for Older Adults
Posted 4 months ago
Vitamin D is a dietary ingredient for bone health, immunity, and possibly cancer defense. It has become nearly ubiquitous in the supplement routines of older adults. But as a recent Medscape exposé, “Vitamin D Overdose: When Good Intentions Turn Toxic,” warns, even this widely hailed nutrient can become dangerous when dosage goes unchecked.
.
The Unexpected Pitfalls of Over-Supplementation
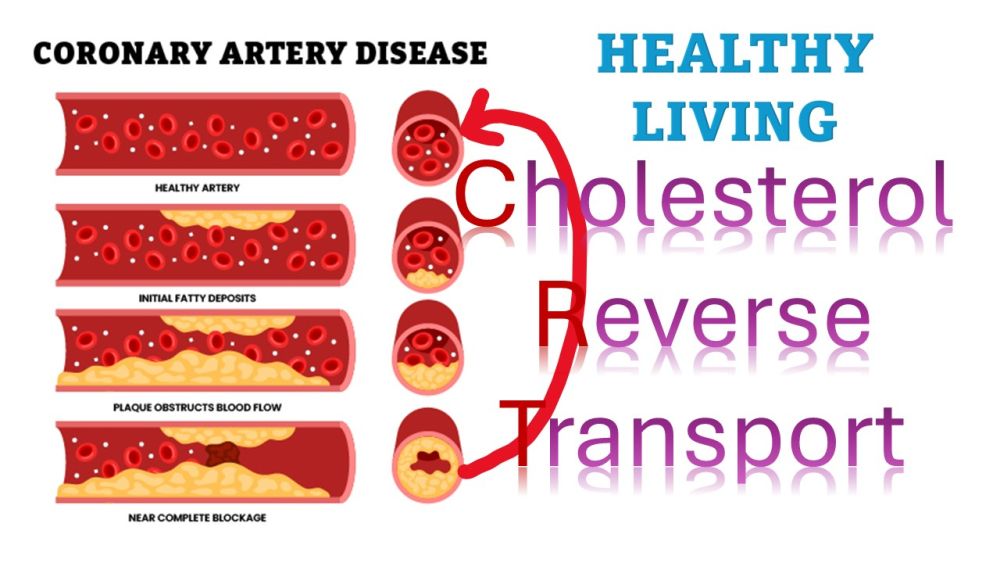
Vitamin D plays a crucial role in calcium absorption and bone integrity. It helps the body absorb calcium, which is essential for maintaining strong bones. However, as the Medscape article underscores, 'good intentions' can lead to hypervitaminosis D, with serious consequences including hypercalcemia, soft-tissue calcifications, and kidney injury.
Supporting this caution, hypervitaminosis D is medically defined by critically elevated blood levels of 25-hydroxyvitamin D, typically above 150 ng/mL, which triggers dangerous calcium buildup in tissues.
Office of Dietary Supplements, while some experts suggest doses up to 10,000 IU may be marginally tolerated under medical supervision
Why Seniors Are Especially at Risk?
Older adults often face a precarious trifecta of risk factors: diminished skin synthesis of vitamin D, restrictive diets, and reliance on supplements to bridge the gap. At the same time, age-related decline in kidney and liver function may impair vitamin D metabolism, increasing susceptibility to toxicity. Many seniors also take medications like thiazide diuretics that can amplify calcium levels, further heightening the risk of hypercalcemia.
Vitamin D in “Old Age”
Excess vitamin D frequently manifests through vague symptoms like fatigue, nausea, constipation, confusion, muscle weakness, and dehydration that mimic age-related ailments, often delaying diagnosis. Other symptoms include frequent urination, appetite loss, and bone pain.
A particularly tragic case from London, where an 89-year-old man died after months of excessive vitamin D (estimated 60,000 IU/day), spotlights the dire consequences. His vitamin D level reached the lab’s maximum, and he suffered fatal hypercalcemia amid pre-existing heart and kidney conditions. This case serves as a stark reminder of the potential dangers of vitamin D overdose, especially in older adults.
Guidelines for Safe Supplementation in Elderly Adults
Health authorities generally recommend that older adults over 70 aim for about 800 IU of vitamin D per day (20 µg), sufficient to maintain bone and muscle strength in most individuals. At the same time, the tolerable upper intake level for the general adult population has been set at 4,000 IU daily (100 µg), beyond which the risk of toxicity rises significantly. While some clinicians may cautiously prescribe higher doses, sometimes up to 10,000 IU daily, for patients with diagnosed deficiency, such regimens should always be supervised and closely monitored through regular blood testing, providing a safety net for your health.
Routine supplementation beyond the recommended allowance is not universally endorsed for otherwise healthy, community-dwelling seniors. In fact, the U.S. Preventive Services Task Force recently issued a D-grade draft recommendation against daily vitamin D (with or without calcium) for fall and fracture prevention, noting a lack of evidence for meaningful benefit. Instead, experts emphasize a holistic approach to bone health: combining moderate supplementation with weight-bearing exercise, balance training, adequate protein and calcium intake, and regular osteoporosis screening.
Ultimately, the safest path for seniors is moderation. A daily intake close to the recommended 800 IU, adjusted based on blood levels of 25-hydroxyvitamin D, offers the benefits of supplementation while avoiding the dangers of hypervitaminosis D. This balance empowers you to take control of your health. Megadoses taken without medical oversight are risky and in some cases, deadly.
Some guidelines allow 1,000 IU/day supplementation in older adults, which is accepted especially for those with limited sun exposure or dietary intake.
Despite the Recommended Dietary Allowance (RDA), the U.S. Preventive Services Task Force (USPSTF) recently issued a draft recommendation giving a D grade for vitamin D (with or without calcium) in fall and fracture prevention among seniors. The USPSTF is an independent panel of experts in primary care and prevention that systematically reviews the evidence of effectiveness and develops recommendations for clinical preventive services. The group cites no proven benefit from supplementation in otherwise healthy, community-dwelling older adults. Instead, it emphasizes physical activity, balance training, and routine osteoporosis screening.
Smart Supplement Strategy for Seniors
Test before supplementing. Monitoring serum 25-OH vitamin D and calcium levels helps tailor dosage and avoid overshoot.
Stick close to the RDA unless otherwise advised. Generally, 800 IU/day is sufficient for those > over 70, with upper limits of no more than 4,000 IU/day.
Vitamin D is just one piece of bone health; exercise, balanced nutrition, fall prevention, and regular medical review are equally vital, especially given recent USPSTF findings.
Conclusion: Sunshine, Supplements, and Sensible Strategy
Vitamin D remains a powerful nutrient, however, it carries risks if misused. Among seniors, particularly vulnerable to both deficiency and overdose, the key lies in precise, individualized supplementation under medical oversight. When used correctly, vitamin D can be a source of hope and health, not in excess, but not in neglect either.