How Gene Therapy Could Change the Future of Huntington’s Disease Treatment
Posted 3 months ago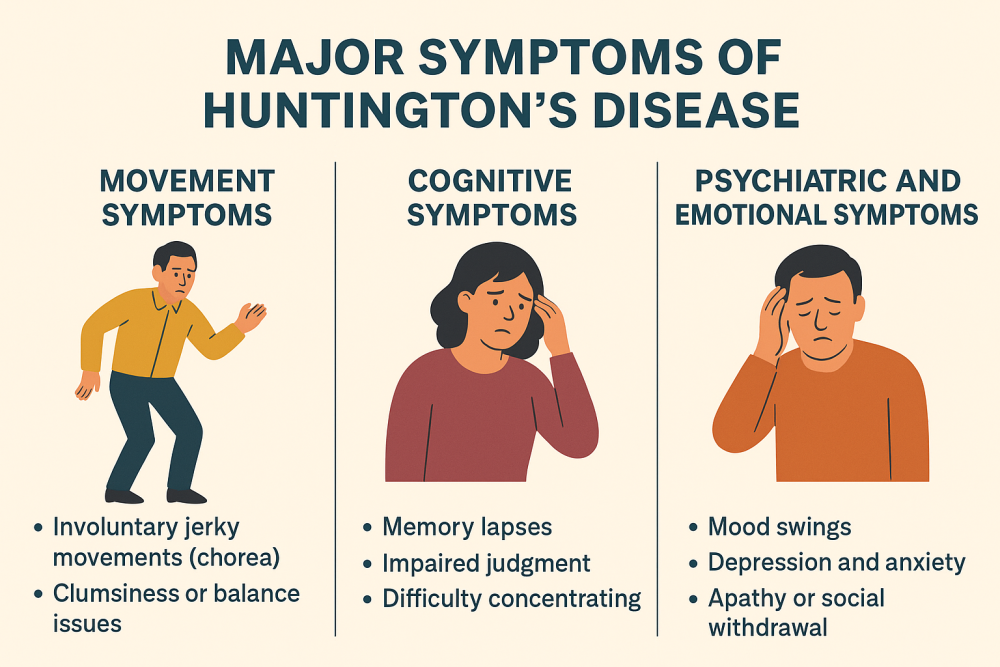
In September 2025, Nature reported a breakthrough that could redefine the Huntington’s disease (HD). For the first time, a gene therapy delivered surgically into the brain showed signs of slowing the progression of HD in humans.
Huntington’s Disease (HD) is an inherited genetic disorder due to a mutation in the Huntingtin (HTT) gene, which contains an abnormal repetition of DNA code. This faulty code forces the body to produce a defective protein called mutant huntingtin, which builds up and damages nerve cells in key brain regions. The damage primarily strikes the striatum and cortex, which control movement, thinking, and emotion. Once the disease begins, the decline is progressive and, tragically, there is currently no cure.
The faulty gene could be transferred from partents to their children. Every child of a parent with HD has a 50% chance of inheriting the faulty gene. Symptoms typically begin between ages 30 and 50, but the genetic clock is ticking from birth. Once triggered, the disease progresses over 10–20 years, often leaving patients bedridden and entirely dependent before premature death.
For decades, treatments have only targeted the symptoms — easing involuntary movements with medications or supporting patients with psychiatric drugs and physical therapy. But these do not touch the underlying genetic cause. The medical challenge has always been: how do you silence the faulty gene?
From Symptom Control to Genetic Precision
Until recently, treatment for Huntington’s disease was limited to short-term symptomatic relief. Drugs for controlling involuntary movements, and antidepressants could ease mood swings. But nothing slowed the relentless march of neurodegeneration.
The first genuine attempt to strike at the disease’s genetic root came from antisense oligonucleotides (ASOs), small strands of DNA designed to reduce the toxic huntingtin protein. Hopes were high. But by 2021, the most advanced trial was halted after failing to show meaningful benefit, a sobering reminder of just how difficult Huntington’s is to treat.
That setback forced scientists to think bigger: instead of repeatedly injecting synthetic molecules into the spinal fluid, what if we could deliver a one-time genetic “fix” directly into the brain?
Clinial Trials Postive Outcomes That Could Change Everything
In September 2025, Nature reported a breakthrough that could redefine the Huntington’s disease (HD). For the first time, a gene therapy delivered surgically into the brain showed signs of slowing the progression of HD in humans.
The trial, meticulously planned and executed, involved 29 participants in the early stages of the disease and tested a therapy developed by uniQure, a biotech firm in Amsterdam. Patients received a single high-dose infusion of the treatment directly into the striatum. Over three years, those treated experienced an average 75% reduction in disease progression compared to controls, based on multiple clinical measures. Even more convincing, cerebrospinal fluid tests showed a significant drop in mutant huntingtin protein.
If validated in larger studies, this would mark the first time a therapy could alter the natural course of Huntington’s, moving beyond symptom management into true disease modification.
How the Therapy Works: A MicroRNA Targets Mutant HTT
At its core, the therapy harnesses the power of gene silencing. Scientists use a harmless viral vector (an engineered adeno-associated virus, or AAV) to carry a piece of genetic code into neurons. That code produces a microRNA (miRNA) molecule that binds to the mutant HTT messenger RNA and destroys it, preventing the production of the toxic protein.
Unlike drugs that fade from the bloodstream in hours or days, the hope is that this genetic “biomedicine” keeps working for years, maybe for life. And because it’s delivered straight into the striatum via stereotactic neurosurgery, the therapy targets the neurons most vulnerable to Huntington’s.
Although miRNA biology has been extensively studied, no miRNA-based therapy has yet been approved for human use. Huntington’s may become the proving ground.
The Promise and the Problem
The data are striking, but not definitive. The trial was small. The procedure is invasive, requiring precision brain surgery. Long-term safety remains uncertain: could the viral vector trigger immune responses or cause unintended gene silencing? And how long will the benefits last — years, decades, or only temporarily?
Moreover, the therapy was evaluated among people with early-stage disease. It’s unclear whether it could help patients who are already further along, or whether it would work best if given before symptoms even begin, a possibility since genetic testing can identify carriers decades in advance.
Implications Beyond Huntington’s
If this therapy proves effective, the positive outcome could extend far beyond Huntington’s. The success of gene therapy in one neurodegenerative disease would open the door to similar approaches for Parkinson’s disease, ALS, frontotemporal dementia, and Alzheimer’s.
The broader lesson is that we are finally learning to treat diseases at their genetic root rather than just patching up symptoms. That shift from managing decline to rewriting destiny represents nothing less than a revolution in medicine.
A Moment of Careful Optimism
For families living under the shadow of Huntington’s, even cautious optimism feels like a breakthrough. For decades, HD has stood as an unyielding symbol of genetic fate. But now, for the first time, there’s a glimpse of hope that a single therapy might change the trajectory of the disease, offering a ray of hope and relief to those affected.
The road ahead will be long. Regulators must carefully weigh risks. Larger trials are needed to confirm benefits. Access and affordability will be significant hurdles. But the fact remains: Huntington’s disease, once considered incurable, may finally be within reach of proper treatment.
In the world of medicine, where progress is often measured in small steps, this seems like a giant leap forward for neurogenetics.




