The Future of Diabetes Care: Treatment Without Daily Injections
Posted 4 months ago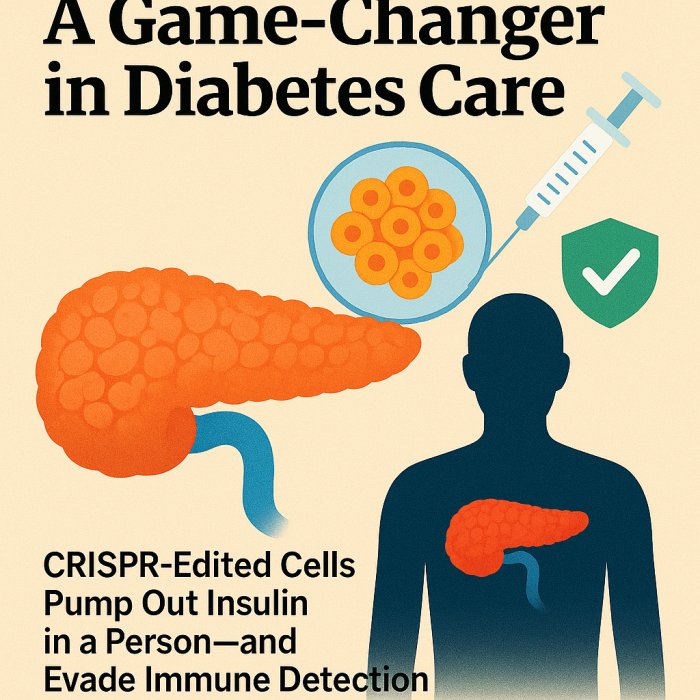
Executive Summary
Scientists have achieved a breakthrough in the fight against type 1 diabetes by using CRISPR gene-editing technology to create insulin-producing cells that can survive in the human body without being attacked by the immune system. In a first-ever trial, these engineered cells were implanted into a patient, where they began producing insulin for several months without requiring daily injections or risky immune-suppressing drugs. While still in the early stages, this discovery offers real hope that millions of people living with diabetes may one day be freed from lifelong dependence on insulin shots and blood sugar monitoring.
Imagine living with type 1 diabetes and suddenly, your life no longer revolves around regular insulin injections, constant blood sugar monitoring, and the fear of dangerous highs and lows. That day may be arriving soon, thanks to a groundbreaking medical milestone achieved just this week.
In what’s being heralded as an actual medical first, scientists have successfully implanted CRISPR-edited pancreatic islet cells, those tiny clusters in the pancreas that produce insulin, into a person with type 1 diabetes. Miraculously, these cells began delivering life-saving insulin for several months. And here's the clincher: the patient didn't need to take any immunosuppressing drugs to stop their body from rejecting the transplanted cells.
Why It Matters?
For decades, the only way to replace lost insulin production has been through islet or pancreas transplants, often from deceased donors. But such transplants come with a steep cost: lifelong immune suppression to prevent rejection, which carries serious risks like infections, cancer, and other complications.
Scientists have found a new path forward that could eliminate those dangers.
How It Works?
Researchers took islet cells from a non-diabetic donor and used CRISPR genetic-editing technology to make two critical changes:
Disable immune-triggering genes: These edits essentially cloak the transplanted cells, preventing them from waving red flags to the immune system.
Add a "don't eat me" marker: Through a viral delivery system, the cells were engineered to express CD47, a protein that tells the body’s natural killer cells to leave them alone.
These cells became invisible to the immune system while performing their vital duty: pumping out insulin like little sugar-regulating workhorses.
Why This Feels Like ‘Hope’?
This isn’t science fiction, it’s real. A real person now has functioning islet cells in their body without the burden of lifelong immunosuppression. The early results are still limited (only one patient so far, with a follow-up of a few months), but the implications? Vast.
What Comes Next?
What Comes Next? Before this becomes a widely available treatment, scientists must test this approach on more patients, follow them over extended periods, and ensure safety at every turn. Large-scale trials are likely down the road, with regulatory approval still to be earned. This rigorous process is in place to ensure the safety and efficacy of this potentially revolutionary treatment, providing confidence and reassurance to all involved.
In Summary
The Breakthrough: CRISPR-edited islet cells implanted in a type 1 diabetic produce insulin for months without immune suppression
The Innovation: Edits remove immune-triggering signals and add CD47 to inhibit immune attack.
The Potential: This treatment has the potential to free patients from insulin shots and risky drugs, marking a monumental shift in diabetes care. It's a potential that inspires and excites, offering a new horizon in the fight against diabetes.
Additional Reading
Hope for diabetes: CRISPR-edited cells pump out insulin in a person – and evade immune detection
Disclaimer
The contents provided on www.biomedglobal.org are intended for general informational and educational purposes only. This website's information, articles, and resources are based on data and findings from scientific publications, publicly available research, and reputable sources.
While every effort is made to ensure accuracy and reliability, Biomed Global does not guarantee, endorse, or assume responsibility for the information's completeness, timeliness, or validity.
The material on this website should not be considered a substitute for professional advice, diagnosis, or treatment. Users are strongly encouraged to consult qualified healthcare professionals, researchers, or subject-matter experts before making decisions based on the information presented here.
Under no circumstances shall Biomed Global, its affiliates, contributors, or authors be held liable for any direct, indirect, incidental, or consequential damages arising from the use of, or reliance on, the content of this website.
By accessing and using www.biomedglobal.org you fully acknowledge and agree to this disclaimer.





